Menopausal symptoms like hot flashes and night sweats get a lot of press, but what about the less discussed symptoms like changes to the genital and urinary tracts? Genitourinary Syndrome of Menopause (GSM) refers to the changes that may occur to the vulva, vaginal, urethra and bladder. Symptoms can include vulvovaginal dryness, burning, itching, irritation, discharge, pain with intercourse, urinary frequency and urgency, and recurrent urinary tract infections. The decline in estrogen around menopause causes thinning of the vulvar and vaginal tissues and changes in the urethra and bladder lining too. There’s less blood flow and less normal vaginal lubrication. The pH of the vagina can change, and women can be more susceptible to vaginal and urinary tract infections. Unlike hot flashes, GSM does NOT get better with time, and it doesn’t get better without treatment. Unfortunately, a lot of women don’t mention this to their medical provider! When they do, they often wait months to years. Because the anatomic changes associated with GSM get worse with time, it can be harder to treat by waiting. But, there are effective treatment options!
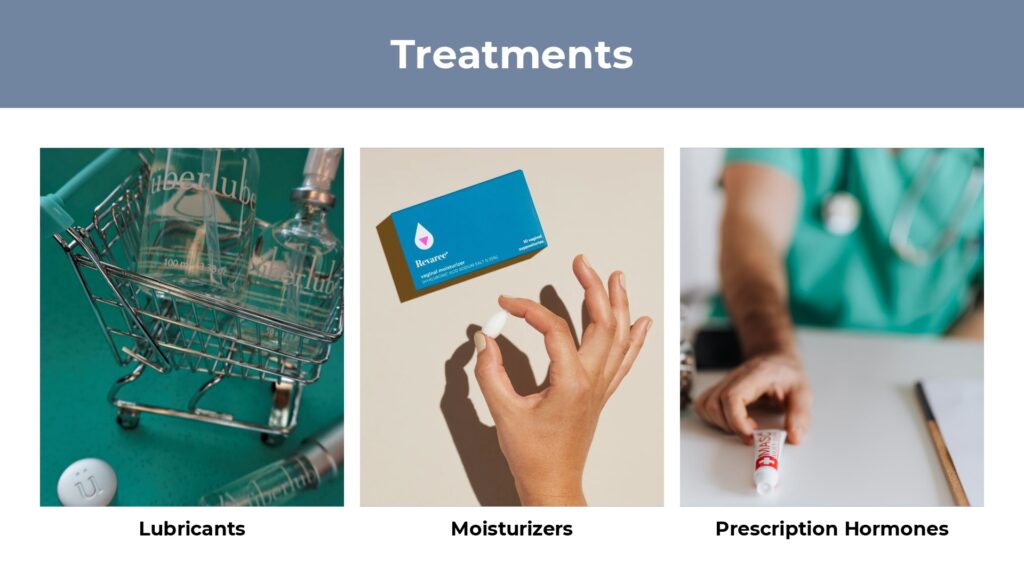
Lubricants can help with dryness during intercourse, and some women will do fine with this alone. Sometimes there’s some confusion about when to use a lubricant and when to use a moisturizer. A lubricant is used for sexual activity with a partner or for self-pleasure—think “L” is for “loving.” I generally recommend trying a silicone-based lubricant like Uberlube or Wet Platinum (just to name a couple) because a silicone lubricant will last longer than a water-based lubricant. Silicone lubricants usually have very few ingredients and don’t affect the pH of the vagina because they don’t contain water. A lot of women do fine with water-based lubricants, but some of the ingredients in them like glycerin may predispose to infections. Water-based lubricants should have a pH and osmolality that is close to normal vaginal conditions like a pH 3.8 to 4.5 and osmolality of 260-370 mosm/kg. Whew, that’s a lot of science for a lube! One company that has lubricants without a lot of additives is Good Clean Love. There are also oil-based lubricants, but these shouldn’t be used with condoms and can increase the risk of infection. Some of my patients with sensitive skin have used coconut oil with good success, but it does have a pH of 7-8, so could theoretically increase the chances of infection. Stay away from warming or flavored lubricants! You can Google lubricants and pH and find a whole list of products and their pH and concentrations.
Moisturizers are used in between sexual activity to try to restore water content to the vaginal tissues and plump them up. Think “M” for “Maintenance.” Most will contain something like hyaluronic acid which is found in a lot of the products we use on our faces to try to diminish wrinkles and plump up our skin as we age. One brand is Revaree which is a hyaluronic acid suppository that should be used 2-3 times weekly. Moisturizers can be ordered online or bought in the store without a prescription. They are nonhormonal and safe for everyone. The North American Menopause Society (NAMS) which is now known as The Menopause Society recommends vaginal moisturizers as first line treatment for GSM.
If you aren’t getting results from these measures, then you should talk to your doctor about local vaginal hormones. There are very few contraindications to using vaginal hormones, but if you have had breast or uterine cancer, then you should talk to your oncologist before using them.
Studies have shown that local vaginal hormones stay local and blood estrogen levels do not exceed a normal postmenopausal range. There are many different forms of vaginal hormones. There are estrogen creams, tablets, inserts, and rings. A lot of women start with estradiol cream or tablets because they have generic prescription options that can be more affordable. The cream or tablet will be inserted in the vagina at bedtime nightly for a couple of weeks and then reduced to twice weekly. Estradiol inserts resemble small capsules that are placed in the vagina at bedtime. There’s also a ring that can be used in the vagina for 90 days at a time.
Two unique types of vaginal therapy are prasterone and ospemifene. Prasterone is a vaginal adrenal hormone suppository that gets metabolized to estrogen and testosterone in the vagina—those vaginal cells are so smart! Yes, we also have testosterone receptors in the lower vagina, urethra, and bladder, so prasterone can help treat these tissues too. Ospemifene is a daily oral medication in a class of medicines known as SERMs (Selective Estrogen Receptor Modulators)—it acts like an estrogen in the vaginal tissues but not in the breast or other areas of the body.
Now, if a woman doesn’t respond to these treatments, especially if her symptoms have been going on for a while or she has narrowing of the vagina, then she may need more intensive interventions. Using vaginal dilators may help gently stretch the vaginal tissues in order to accommodate vaginal intercourse if that is her desired goal. Pelvic physical therapy may be needed to help learn how to relax the pelvic floor muscles to break the pain cycle. If having sex has been painful for a while, then of course, the body tries to protect itself from pain and can react with muscle spasms and tightening. Sometimes counseling or sex therapy may be necessary if there’s an emotional component or relationship issues.
As you see, there are A LOT of treatment options for GSM. Don’t suffer in silence! Talk to your gynecologist about your concerns. You can find a directory of menopause specialists in your area at menopause.org if you are not getting the help you need!
This post is for informational purposes and is not medical advice.

